1. Patient Complaint & History
Jane (gravida 0, para 0) and John have been trying to have a baby for a long time. They are delighted when Jane does a home pregnancy test and it indicates positive. She schedules an appointment, and she has come to the Obstetrics clinic for her first check-up and to confirm the pregnancy, approximately 8 weeks since she took the test.
2. Exam
First Trimester Testing
First-trimester screening is performed. Genetic Screening is undertaken.
A triple screen is performed including a maternal serum alpha-fetoprotein (MSAFP), beta human chorionic gonadotropin hormone (hCGH), and unconjugated estriol (uE3). An ultrasound was also performed.
3. Lab Results:
Although the estriol value is normal, Jane’s MSAFP is slightly elevated and at 3.0 MoM (3.0 Multiples of the median) and her hCGH level is 1200 mIU/mL (over 50% higher than expected for a single birth). An ultrasound shows that Jane as an amniotic fluid index (AFI) of 25 indicating early polyhydramnios <24). However, it is difficult to assess the ultrasound due to poor resolution.
Table 1. Reference blood markers and fetal condition.
| Condition | MSAFP | uE3 | HCG |
| Neural tube defect | Increased | Normal | Normal |
| Trisomy 21 | Low | Low | Increased |
| Trisomy 18 | Low | Low | Low |
| Trophoblast pregnancy | Low | Low | Very High |
| Multiple gestation | Increased | Normal | Increased |
| Stillbirth (fetal death) | Increased | Low | Low |
- In a normal pregnancy, between 28-32 days, the embryo is changing from a flat disk to a tubular structure.
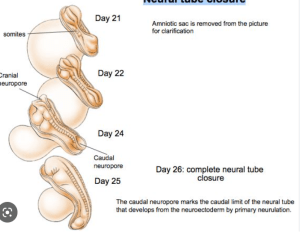
- By 28-38 days the normal embryo looks like this
4. Follow-up Appointment Tests
Jane was instructed to return at 12 weeks for another ultrasound and further 2nd-trimester testing.
Another ultrasound is taken and amniocentesis is performed. A doppler echocardiogram is conducted. Additional blood values are also assessed.
5. Follow-up Results
A blood sample from Jane is obtained and a value of 380 ng/mL for alpha-fetoprotein (AFP, 0-40 ng/ML is normal) is determined. Normal serum levels of AFP are 10-20 ng/mL. Levels rise during pregnancy reaching a peak level at the end of the first trimester but they become diluted due to fetal blood volume increases. Substantial levels are found in 90% of neural tube defect cases.
An amniocentesis is scheduled to confirm an elevated level of AFP in the amniotic fluid.
The doppler indicates two heartbeats, indicating to the obstetrician that there are 2 babies, but there is a problem. Twin A is normal, but Twin B appears to have a major anatomical birth defect.
- Let’s review medical scans of anatomical features.
Review osteology starting at the feet and ascend. Check lower limb bones; pelvis, vertebral column. Then observe cervical region and skull. Note deficiencies.
Model of the surface of the baby
Model of the skeletal system
A model of an encephalocele
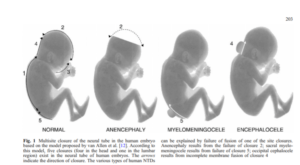
Schematic of a neural tube defect
DeMarco et al., 2006 Neurogenetics 7:201-221
Model of a normal fetal skull
Segmented model of the brain
Photogrammetry specimen of a brain
- JAMBOARD
Question 1: What is polyhydramnios and what can it indicate?
A. Too little amniotic fluid and a chromosomal defect such as Trisomy 21.
B. Too little amniotic fluid and a chromosomal defect such as Trisomy 18.
C. Too little amniotic fluid and the presence of twins.
D. Too much amniotic fluid and a neural tube defect.
Question 2: What anatomical structures are deficient in Twin B and what is this condition called?
A. Nerve tissue -Encephalocoele
B. Brain tissue -Anencephaly
C. Cardiac Tissue – Dextrocardia
D. Osseous Tissue – Sirenomelia
- GROUP DISCUSSION FOR Questions 1 and 2
Case Scenario Continued:
The parents begin considering possible options. This begins a series of emotional discussions between the parents that consider religious beliefs, family values and future extended family ramifications as well as immediate and future health issues. They immediately seek the advice of their Ob/Gyn.
- JAMBOARD
Question 3: Upon diagnosis, what possible decisions might the parent suggest to you as their physician?
A. Terminate the pregnancy completely.
B. Terminate the anencephalic twin only.
C. Bring both to term.
D. Any of the above, but depending on the state.
- GROUP DISCUSSION for Question 3
Case Scenario continued:
The parents undertake extremely emotional discussions realizing that whatever decision they take will likely have consequences that they will live with for many years. Conflicting emotions will likely arise, for example, the parents may feel excited about the healthy twin, but sad about the one that they know will not survive
Ultimately, the parents agree that they cannot terminate and decide to maintain the pregnancy and “let nature take its course.” Mom begins to feel the movements of both twins and mentions that she is feeling an emotional bond develop. Another ultrasound scan is performed at 20 weeks.
Return to the sketchfab model here:
Both twins are moving and displaying reflexive muscular movements. However, the parents are very alarmed by the appearance of the craniofacial region, characterized by protruding eyes as well as the absence of a forehead and calvaria, thus leading to questions about the basic cognitive ability of the infant.
- JAMBOARD
Question 4: An infant born without a brain (anencephalic) should not be afforded human rights.

GROUP DISCUSSION FOR Question 4
Case Scenario Continued:
As the pregnancy continues and the parents learn more about anencephaly, they begin to consider the possibility of organ donation from Twin B. They begin to embrace the idea that their infant could potentially be an organ donor and raise the idea with the physician. Their reason is that their infant could help another in need of an organ donation and provides a sense of human value.
They raise this option with their physician who must act in the best interest of the infant, but also provide the best level of care possible for the mother.
- JAMBOARD
Question 5: It is ethically acceptable to obtain organs from a newborn infant with a lethal condition following death.

GROUP DISCUSSION FOR Question 5
Case Scenario continued:
The amnion breaks and Twin A is born takes a breath, the umbilical cord is cut and the baby is given to the mother to hold. Twin B is born immediately afterward, and the umbilical cord is cut and also given to the mother to hold. However, Twin B quickly begins pulmonary distress.
- JAMBOARD
Question 6: Twin B should be ventilated to support his life for the purpose of organ retrieval and donation?

Question 7: There are limits to what the team can do to keep the baby alive in the short term for the sake of organ donation.

GROUP DISCUSSION FOR Questions 6 & 7
Case Scenario: Epilogue
The hospital ethics committee convened to determine whether invasive ventilation could be used to maintain Twin B’s life while a recipient was found. The response was:
- Placing a baby on life support for the express purpose of organ retrieval is not ethically acceptable, but this also can also apply to life support for the purpose of family members meeting the baby and/or religious ceremonies.
- If the family wants the donation & doctors agree that ventilation would be limited so that pain and suffering was absolutely minimal, then there could be an exemption.
The amnions broke 6 weeks premature. Both babies were born and births were largely unremarkable. Mom held both twins. Photographs were taken together. Anencephalic oxygen level began dropping precipitously at postpartum hour 3. Twin B was given some sedation and ventilated. Parents were in the ICU with both babies who were baptized. However, no suitable recipients were found. Twin B was taken off the ventilator and passed 12 hours later.
